Disclaimer: This article is intended for informational and educational purposes only. It is not a substitute for medical, psychological, or professional advice. Readers experiencing emotional distress should seek help from a qualified healthcare or mental health professional.
When the Healer Hurts: The Hidden Emotional Toll of Patient Loss in Medicine
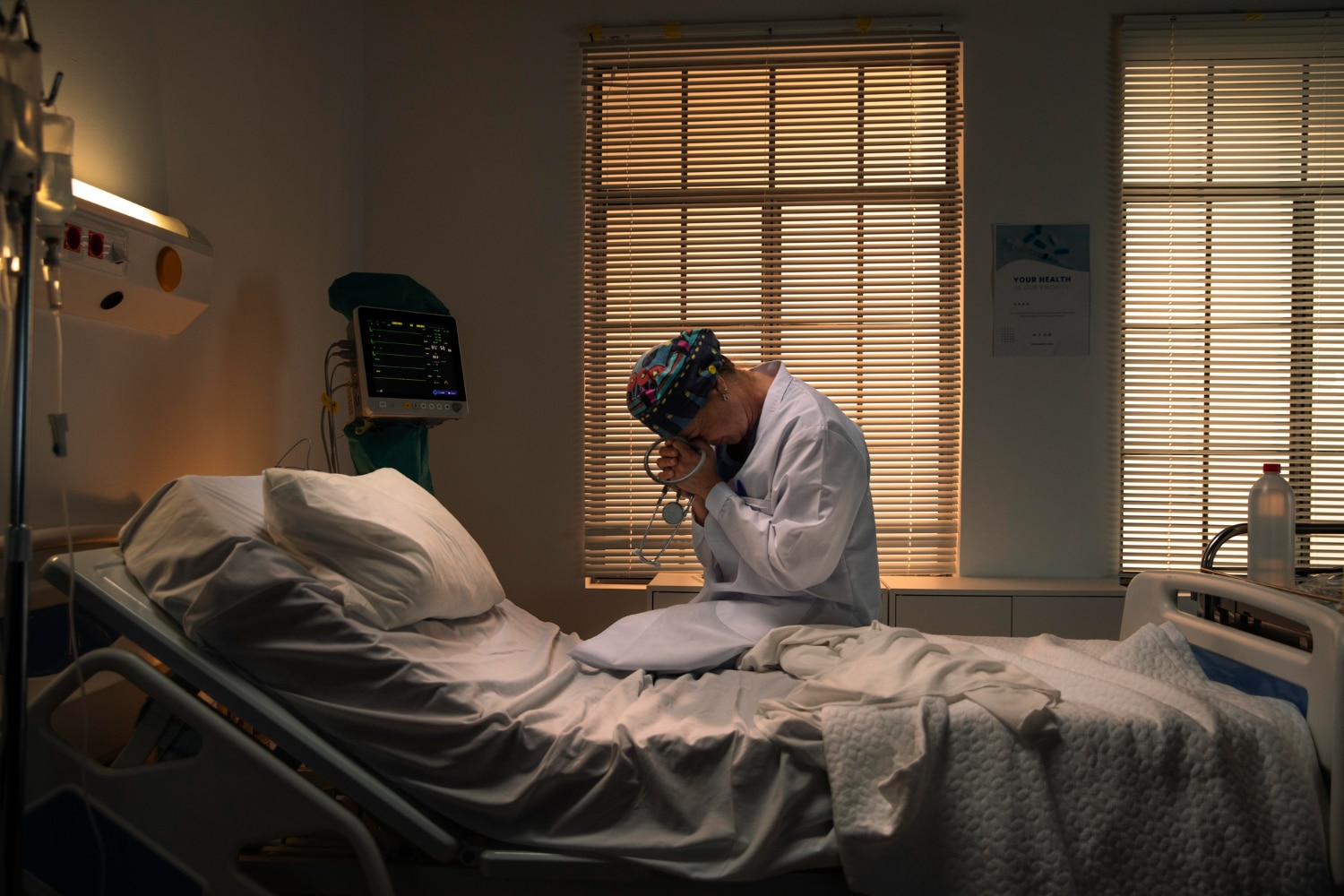
It is a photograph that has resonated deeply across the world: a doctor crouched outside a hospital, head in his hands, visibly overwhelmed after losing a young patient. The moment, captured outside a California hospital, quickly spread across social media—not because of its drama, but because of its honesty. Behind every life-saving procedure and confident diagnosis lies a human being who also feels the weight of loss.
In an era when medical professionals are often seen as resilient and untouchable, this image reminded millions that behind the white coat is a person—one capable of deep compassion and grief.
This article explores the emotional impact of patient loss on healthcare workers, drawing on verified data and peer-reviewed research to understand how doctors process grief, why the stigma around vulnerability persists, and what changes could help protect the mental health of those who care for others.
The Unseen Emotional Weight of Saving Lives
Doctors, nurses, and emergency medical staff regularly stand at the intersection of life and death. Every shift brings unpredictable challenges—critical cases, emergencies, and, at times, devastating losses. While the public naturally empathizes with grieving families, the emotional toll on the healthcare professionals delivering that tragic news often remains invisible.
According to the National Academy of Medicine (NAM), physicians experience higher rates of emotional distress and burnout than most professions. The 2022 Journal of Emergency Medicine reported that nearly 60% of emergency physicians exhibit symptoms consistent with burnout, while approximately 30% show signs of post-traumatic stress due to repeated exposure to trauma and death.
When a young patient dies unexpectedly, the impact is even more profound. “There’s no amount of training that prepares you for the death of someone with their whole life ahead of them,” said one emergency physician interviewed by The American Medical Association (AMA). Such cases often challenge not only medical skill but also emotional endurance.

The Hidden Stress of Emergency Medicine
Emergency departments operate in a constant state of urgency, where seconds can determine outcomes. Physicians must make rapid, life-altering decisions, often with limited information and no prior relationship with the patient. This intense environment leads to what psychologists call secondary traumatic stress or vicarious trauma—a condition where caregivers absorb the emotional weight of the crises they witness.
A 2021 study in The Western Journal of Emergency Medicine found that repeated exposure to traumatic events significantly increases the risk of emotional exhaustion and detachment among ER staff. Over time, these pressures can manifest as burnout, anxiety, or depression.
Despite this, many doctors feel compelled to maintain composure. The culture of medicine has long emphasized emotional restraint—a belief that detachment is essential for clear decision-making. However, experts now warn that chronic suppression of emotion can have long-term mental health consequences.
The American Psychological Association (APA) notes that while emotional regulation is important, “denying emotional responses altogether can lead to psychological strain, decreased empathy, and professional fatigue.” In short, being stoic may help doctors function during emergencies, but it can also isolate them afterward.

When the Patient Is Young
The death of a young patient, such as a teenager or college-aged individual, presents a unique kind of heartbreak. These moments violate the natural order—when youth and vitality meet sudden loss. For healthcare providers, this can trigger feelings of helplessness, guilt, or moral distress.
Dr. Louise Aronson, in her New England Journal of Medicine essay, wrote that the loss of a young patient “pierced the professional shield I didn’t even know I’d built.” Such experiences remind clinicians that, despite years of training, medicine has limits. Even the best care cannot always prevent tragedy.
These moments often stay with doctors for years. As many medical professionals have shared, some patient losses remain vivid long after others fade—especially when the patient reminds them of their own family or when the outcome feels unjust. This lasting emotional imprint is part of what the Journal of General Internal Medicine describes as the “moral residue” of caregiving.

Who Heals the Healers?
While doctors are trained to heal others, their own healing is often overlooked. Studies show that physicians face disproportionately high rates of depression and suicide compared with the general population.
The National Academy of Medicine (NAM) reports that physician suicide rates are more than double those of the general public for women and 1.4 times higher for men. Factors include high workload, lack of sleep, emotional exhaustion, and stigma surrounding mental health.
That stigma runs deep. Many physicians fear that seeking counseling could jeopardize their medical license or reputation. According to a 2023 AMA survey, nearly 40% of doctors avoided mental health services out of concern that disclosure might affect their professional standing.
This reluctance has serious consequences. Without adequate emotional support, grief and burnout can escalate into long-term mental health conditions. As Dr. Lorna Breen Heroes’ Foundation advocates, healthcare systems must establish confidential, stigma-free avenues for doctors to seek help—because caring for those who care for others is not optional; it’s essential.

Changing the Culture of Medicine
In recent years, hospitals and medical organizations have begun addressing the emotional realities of patient loss more openly. Programs such as peer support networks, resilience training, and mental health hotlines have emerged across the U.S., aiming to give healthcare workers safe spaces to process their emotions.
For instance, the Mayo Clinic’s “Healing the Healer” program provides confidential debriefing sessions after traumatic cases, while the Cleveland Clinic’s Caregiver Support Team offers 24/7 emotional support for staff dealing with loss. These initiatives recognize that emotional wellness directly affects patient care, professional performance, and retention within the medical field.
However, experts agree that institutional change must go further. Structural reforms—such as reducing excessive administrative workloads, ensuring adequate staffing, and normalizing psychological counseling—are vital to preventing burnout at its roots.

Recognizing Humanity in Healthcare
The viral image of the grieving doctor resonated globally because it exposed something rarely seen: the vulnerability behind the profession. It symbolized the emotional cost of saving lives and the resilience required to face loss repeatedly.
Doctors are not immune to the same emotional spectrum as their patients. They grieve, they question, and they carry memories of those they could not save. Acknowledging that humanity does not diminish their professionalism—it enhances it.
As Harvard Medical School ethicists note, compassion fatigue is not a sign of weakness but a symptom of overexposure to suffering without adequate recovery time. By fostering compassion for caregivers, both institutions and the public can help sustain the empathy that makes medicine humane.
Toward Shared Healing
Ultimately, the story behind that image is not about failure—it’s about shared humanity. It invites a shift in how society views healthcare workers: not as unbreakable heroes, but as individuals performing emotionally demanding work under extraordinary pressure.
Supporting them means creating systems that value mental wellness as much as clinical excellence. It means listening when doctors say they’re struggling and providing resources before crisis strikes.
When we honor the emotional labor of healthcare, we also strengthen the foundation of compassionate medicine. Healing, after all, is a shared act—between patient and doctor, between caregiver and community.
Sources (verified and reputable):
-
National Academy of Medicine (NAM), Taking Action Against Clinician Burnout (2021)
-
The American Medical Association (AMA) Physician Health Report (2023)
-
Journal of Emergency Medicine (2022), “Burnout and Secondary Trauma in Emergency Physicians”
-
New England Journal of Medicine (2018), “The Emotional Toll of Patient Death” – Dr. Louise Aronson
-
Western Journal of Emergency Medicine (2021), “Vicarious Trauma in Emergency Care Providers”
-
Mayo Clinic: Healing the Healer Program
-
Cleveland Clinic: Caregiver Support Resources
-
Harvard Medical School Center for Bioethics

